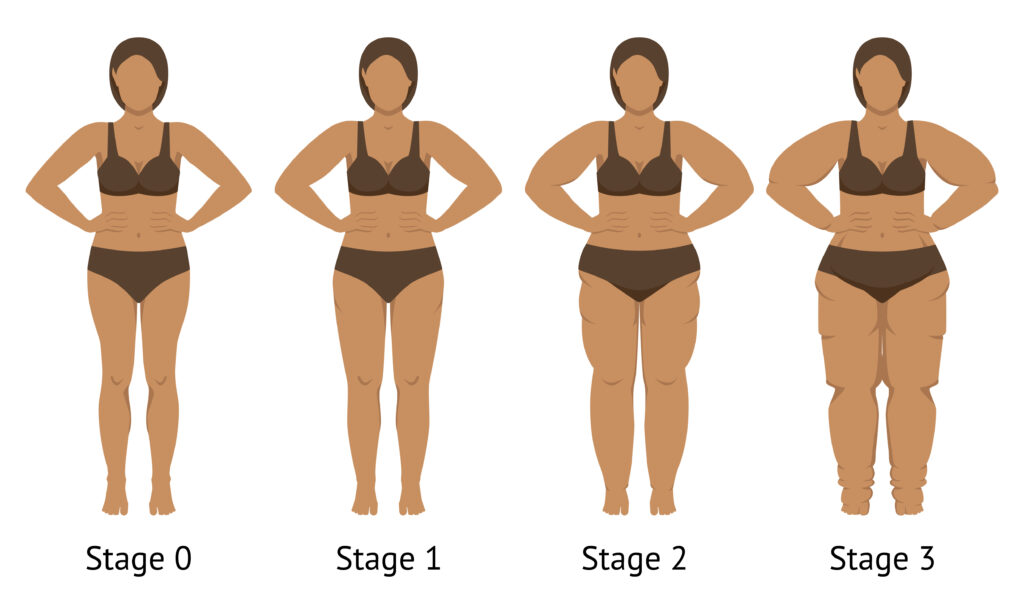
Lipedema is a chronic condition characterized by disproportionate accumulation of adipose tissue, primarily in the lower extremities and sometimes the arms, often accompanied by pain, easy bruising, and mobility issues. It predominantly affects women and is frequently misdiagnosed as obesity or lymphedema. Management focuses on symptom relief, improving quality of life, and slowing progression, as there is no cure. Treatment is typically multimodal, combining conservative strategies, surgical options when necessary, and emerging therapies.
Conservative Therapies
Conservative treatments are the cornerstone of lipedema management, emphasizing non-invasive methods to reduce swelling, pain, and inflammation while supporting overall health. These are often grouped under Complete Decongestive Therapy (CDT), which integrates multiple elements for optimal results.
- Manual Lymphatic Drainage (MLD): This specialized gentle massage technique stimulates lymphatic flow, reduces fluid buildup, and alleviates pain and swelling. It is most effective when performed by trained therapists and combined with other therapies like compression. MLD can break up fibrotic tissue in advanced cases and is a key component of CDT.
- Compression Therapy: Medical-grade garments, such as flat-knit stockings or sleeves (typically 20-30 mmHg pressure), provide graduated pressure to minimize edema, support limb shape, and improve venous and lymphatic return. Custom-fitted options are recommended for better compliance and efficacy. Compression is essential daily and often used post-MLD to maintain benefits, though adherence can be challenging due to discomfort.
- Exercise and Physical Activity: Low-impact activities are encouraged to enhance lymphatic drainage, mobility, and overall well-being without exacerbating symptoms. Options include swimming, water aerobics (leveraging hydrostatic pressure for natural compression), walking with compression garments, recumbent cycling, yoga, Pilates, Chi Gong, Tai Chi, and strength training with light resistance. These help manage weight, reduce inflammation, and improve strength, though they do not directly reduce lipedema fat.
- Nutrition for Healthy Lifestyle: While lipedema fat is resistant to traditional weight loss, anti-inflammatory diets (e.g., Mediterranean-style with omega-3s, antioxidants from leafy greens, berries, and fatty fish) may potentially reduce symptoms and prevent comorbidities like diabetes. Ketogenic or low-carbohydrate approaches have shown benefits in reducing swelling, pain, and weight in some cases. Hydration with minerals, avoiding processed foods, eliminating potentially harmful seed oils (butter, avocado and olive oil, coconut oil, and tallow are generally safe), and attempting to limit exposure to oxalates, histamines, and lectins are key. Weight stabilization is prioritized over aggressive loss.
- Supplements: Various supplements may support symptom management, though evidence varies. Examples include selenium (reduces swelling and infection risk), bioflavonoids (strengthen blood vessels), horse chestnut seed extract (treats venous issues), quercetin (regulates blood pressure), pycnogenol (antioxidant effects), N-acetyl cysteine (prevents tissue damage), butcher’s broom (reduces leg swelling), co-enzyme Q10 (antioxidant), alpha-lipoic acid (fights free radicals), milk thistle/dandelion root (liver support), and systemic enzymes like Wobenzyme (reduce fibrosis). Always consult a healthcare provider and pharmacist before starting.
- Skin Care and Breathing Exercises: Gentle moisturizing with fragrance-free products prevents infections, while deep breathing activates the diaphragmatic pump to aid lymphatic circulation and reduce stress.
- Pneumatic Compression Devices: Home-use inflatable garments connected to pumps provide intermittent compression to move lymphatic fluid, offering an alternative or adjunct to manual methods for controlling swelling and pain.
- Healing Gut Microbiome: Establishing a healthy community of organisms in your gut is critical for overall health and well-being. Raw cultured foods such as kimchi and saurkraut are helpful. Cultured dairy products that promote a healthy gut microbiome include unsweetened Greek yogurt and kefir. Sour dough bread is made with a live culture of L. Reuteri; and L. Reuteri can also be taken as a supplement. Newer research points to supplementation by such organisms as Akkermansia muciniphila, Lactobacillus crispatus, and L. gasseri.
are key to thriving with Lipedema
Dr. Darleen Claire Wodzenski, MS ESE, MA CMHC, PhD, NCC, LPC, ACS is licensed as a Professional Clinical Mental Health Counselor in Florida, Georgia, and Virginia and has personal experience as a thriver with Lipedema. She additionally offers some non-clinical services including Quantum Success Hypnotherapy across the country and internationally. She is also a credentialed massage and neuromuscular therapist with extensive experience in lymphatic clearing. You may reach her at +1 (770) 686-0894 or DrDarleen@orchardhumanservices.org
Emerging Therapies
Research is ongoing for novel approaches, as no pharmacotherapy is approved specifically for lipedema.
- Pharmacotherapy: Agents like metformin and resveratrol (anti-fibrotic/anti-inflammatory), diosmin (reduces venous swelling), selenium (improves inflammation), and sympathomimetics (promote lipolysis). Avoid diuretics that may worsen issues.
- Advanced Devices and Imaging: Pneumatic compression for home use; diagnostic tools like MR lymphography, ultrasound, and bioimpedance for better treatment planning.

therapeutic activity of daily living to
support thriving with Lipedema.
Multidisciplinary Approach
Effective management involves a team including physicians, therapists, nutritionists, and mental health professionals for holistic care. Patient education, goal setting, and psychosocial support are vital to address emotional impacts and improve adherence. Early intervention and tailored plans based on stage and comorbidities are recommended.
Conclusion
Lipedema management requires a personalized, comprehensive strategy starting with conservative therapies to control symptoms, escalating to surgery if needed, and incorporating emerging options as research advances. High-quality studies are essential for evidence-based guidelines. Patients should consult specialists for individualized plans to optimize outcomes and quality of life.
Dr. Darleen Claire Wodzenski, MS ESE, MA CMHC, PhD, NCC, LPC, ACS is licensed as a Professional Clinical Mental Health Counselor in Florida, Georgia, and Virginia and has personal experience as a thriver with Lipedema. She additionally offers some non-clinical services including Quantum Success Hypnotherapy across the country and internationally. She is also a credentialed massage and neuromuscular therapist with extensive experience in lymphatic clearing. You may reach her at +1 (770) 686-0894 or DrDarleen@orchardhumanservices.org
This discussion about the management of Lipedema is for informational purposes only. Consult with your medical, mental health, holistic, and pharmaceutical professionals for guidance and recommendations.
Copyright 2025 PNE Institute, LLC. All rights reserved.